“Personal Health Systems Foresight” was launched as part of the 7th EU Framework Programme to explore options for integrating Personal Health Systems (PHS) into the health care system and to investigate framework conditions required for the Europe-wide introduction of PHS. Furthermore, the project wanted to initiate a mobilisation of the innovation landscape, increase networking, and develop strategies to promote PHS across Europe.
Personalised Health Systems: Chances of a Holistic Approach
Rising costs, an ageing population and a shortage of health care professionals are only three of the numerous challenges Europe’s health system has to face. Personal Health Systems (PHS) promise more individual, effective and efficient health care as they assist in the provision of continuous, quality controlled and personalised health services. PHS are technical aids which gather, monitor and communicate physiological and other health-related data via stationary, portable, wearable or implantable sensor devices. Individual treatments or nutritional advice can then be provided virtually anywhere. Furthermore, PHS technologies can provide new business opportunities and can mobilize novel cross-disciplinary and -sectoral innovation partnerships.
There are already various technically advanced solutions available in the fields of e-health, mobile health and ambient assisted living. Several initiatives have been launched across Europe to increase the integration
of new technologies into the health care system. However, most of these projects are limited to small-scale applications and do not situate PHS within the wider health and social care service systems as they were mostly driven by a technology push. The EU project “Personal Health Systems Foresight” wants to fill this gap by looking at the integration of PHS into the health care system from a more holistic view.
Structure of the PHS Foresight
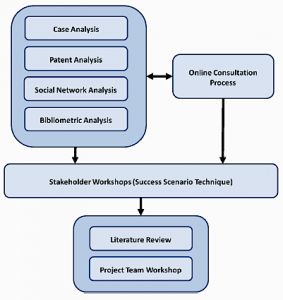
As a first step of the project the team conducted a set of analyses in order to get an overview of the PHS area. These include a bibliometric and a case study analysis to gain information about the present state of the topic, a patent analysis in the field of PHS, and a social network analysis to visualize R&D collaboration networks and central actors in the area of PHS on the European level. Additionally, the project partner developed an online platform in order to generate and cluster visions on related innovations and societal challenges.
On the basis of the results from the analyses and the online consultation process, two stakeholder workshops were organized in order to explore the pathways for desirable future developments. The applied method was the “success scenario” technique, which is described in the following by the example of the second scenario workshop for the PHS foresight, held in Manchester in February 2014.
The Success Scenario Method as Core Element of the Foresight Process
The “success scenario” method can be regarded as a mixed form of conventional scenarios and roadmapping. The latter is often a process that extends upon several workshops and produces highly detailed information relevant to one specific goal. In comparison the success scenario approach usually speeds things up by creating a less structured pathway. It identifies a plausible and desirable course of development, the steps required to receive it and the indicators of progress in the right direction.
A product of the process is the scenario text, which can be used to share the vision and mobilise other actors, but the scenario process itself also has a number of functions including:
- Providing a platform to create mutual understanding and sharing of knowledge,
- forming a stretch target to think beyond the boundaries of “business as usual”,
- developing indicators to move the scenario beyond vague aspirations and produce clarity as to what precisely should be discussed and how goals can be achieved, and
- developing action points and setting priorities.
In this sense the second stakeholder workshop as a core element within the PHS foresight (figure 1) developed elements of a vision for PHS in the year 2030 through a series of steps, in which major dimensions of change, indicators that might be used to assess progress towards desirable outcomes, and actions and strategies to facilitate PHS development in desirable directions were considered. The attainable future could thereby vary across different European countries.
Figure 1: Methodologies applied in the PHS Foresight
The workshop was structured as follows:
- Introduction of participants, overview of project and the PHS area, explanation of the workshop
- Presentation of PHS scenarios (from previous workshop)
- Discussion of success scenario method
- Specification of indicators of success
- Discussion of how far success might be realised in terms of these indicators
- Identification of challenges to be overcome to achieve progress along these lines
- Possible issues affected by these developments
- Key actions required to achieve progress
Indicators, Issues and Strategic Actions for the Implementation of PHS
After an introduction of the participants and a first overview of the project and the PHS area, the PHS scenarios from previous workshop were presented. The participants built 4 break-out groups (BOGs):
a) chronic conditions, b) active independent living, c) acute conditions, and d) healthy lifestyles. These groups discussed what might constitute the success scenario and what specific outcome indicators could be appropriate to illustrate it. The indications from the BOG discussions were further analyzed and refined by the participants, this time in plenary. The resulting list of indicators is presented in table 1.
Table 1: Final set of outcome indicators for the PHS success scenario
Note: The percentages in parentheses after several items are the views of that group as to the extent to which this indicator is liable to have developed by 2030. |
For the next step in the workshop, the participants worked in five BOGs, each focusing on particular areas where transformations may be required for the realisation of the success scenario for PHS. These areas of transformation were defined as:
- Technologies, platforms, infrastructures, technical standards, and research and development
- Data, privacy and public awareness, attitudes and behaviour
- Skills, new occupations, changing new occupational roles and specialisms, training
- Health and social policy, goals and philosophy, funding and financing
- Public-private roles & relationships, changing organisational forms, new business models
The five BOGs then identified issues related to the implementation of PHS in the health care system and finally considered strategic actions relevant to different stakeholders, in the light of these issues.
Strategic actions in relation to interoperability, standardisation and regulation include for instance harmonisation of healthcare systems regulations, interoperability of IT systems, development of common dictionaries and use cases, standards development, legislation for data security and data access.
Actions in relation to developing a PHS innovation eco-system include the coordination and collaboration among a variety of actors in the research, and business communities engaging also societal actors by applying user-centred innovation approaches.
Creating a PHS market with wide accessibility and affordability requires the establishment of market and competition mechanisms and regulations, procurement, development of plans for stage-gated deployment of reimbursement models. Establishment of value chains from priority setting, selection of technologies, to manufacturing and implementation is important and the production of user-friendly and cheap products and services is relevant.
Strategies towards raising social awareness and increasing PHS skills involve actions like educational programmes to introduce PHS systems to professionals and informal carers but also schools, setting up PHS help and advice lines, or incentives to educational institutions to develop PHS strategies and programmes.
PHS research should target to demonstrate PHS benefits and certify PHS products and services. Demonstration of benefits could be done through creation of modelling labs for PHS applications, or building a catalogue of what is available, what is being developed and what needs to be developed through a gap analysis and towards the jointly defined PHS vision. Longitudinal health studies, health economics and cost-effectiveness studies could be deployed along with health technology assessment.
Finally, PHS research should also deal with big data analysis issues while being oriented towards developing customised, user friendly and certified applications easily accessible online and offline. The target groups should be patients, as well as informal carers in the first instance; at later stages the whole of society should be addressed, as there is a need to shift from a reactive to proactive healthcare approach promoting healthy living. The role of EU institutions could be important in supporting PHS research, as well as in providing platforms for disseminating results helping to draw the lessons from both success stories and failures.
Towards a More Individual and Efficient European Health Care System
In summary there was a general consensus among workshop participants that PHS can contribute to improved health outcomes as well as increasing the efficiency of health services. The process of implementing PHS will involve numerous stakeholders in order to build what participants described as a PHS „innovation eco-system”. It will be important to recognise the interests of different stakeholders in order to avoid a decline in health outcomes, to maintain and extend the equity and social inclusion elements of health systems, to stimulate the development of innovative and effective health interventions and medical technologies, to maintain professional competences and social status, to reward entrepreneurial behaviour, and to use and protect personal data.
Meeting these challenges will require experimentation, dialogue, and monitoring of change. Major aspects of change range from the creation of new business models and partnerships between different kinds of organisations, through stimulating the acquisition of new skills and the emergence of new professions in health and health-related workforces. It will also be important to put regulatory frameworks into place that can allow for informed acceptance of evidence-based solutions.
In all of these aspects of change, public attitudes will need to be taken into account, since citizens are crucial stakeholders in these processes. Further development of visions of the desirable futures that can be achieved, and awareness of the problems that may be encountered and the ways in which these may be addressed, will be necessary in the future. The PHS foresight and the results from the success scenario workshop can be regarded as one step in the direction of adopting a holistic and combined approach in understanding PHS and establishing and sharing visions of the desirable futures that can be achieved through the implementation of PHS into the European health care system.
| Authors: | Susanne Giesecke (susanne.giesecke@ait.ac.at), Doris Schartinger (doris.schartinger@ait.ac.at), André Uhl (andre.uhl@ait.ac.at), Totti Konnola (totti.konnola@if-institute.org), Laura Pombo Juárez (laura.pombo@impetusolutions.com), Ian Miles (ian.miles@mbs.ac.uk), Ozcan Saritas (ozcan.saritas@mbs.ac.uk), Effie Amanatidou (effie.amanatidou@mbs.ac.uk), Günter Schreier (guenter.schreier@ait.ac.at) | ||||
| Sponsors: | European Union’s Seventh Framework Programme (FP7 2007-2013) | ||||
| Type: | European Foresight Project | ||||
| Organizer: | Austrian Institute of Technology AIT, Susanne Giesecke, susanne.giesecke@ait.ac.at | ||||
| Duration: | 2012 – 2014 | ||||
| Budget: | 450,000 € | ||||
| Time Horizon: | 2030 | ||||
| Date of Brief: | March 2016 | ||||
Download EFP Brief No. 261: Personalised Health Systems Foresight – the Success Scenario Method
Sources and References
This brief is based on the following report, in which the findings are discussed in more detail:
Amanatidou, E., Miles, I., Saritas, O., Schartinger, D., Giesecke, S., & Pombo-Juarez, L. 2014. Personal Health Systems: A Success Scenario. Personal Health Systems Foresight.
References
Schartinger, D., Miles, I., Saritas, O., Amanatidou, E., Giesecke, S., Heller-Schuh, B. Pompo-Juarez, L., & Schreier, G. 2015. Personal Health Systems Technologies: Critical Issues in Service Innovation and Diffusion. Technology Innovation Management Review, 5(2): 46–57. http://timreview.ca/article/873
Schartinger, D., Miles, I., Saritas, O., Amanatidou, E., Giesecke, S., Heller-Schuh, B. Pompo-Juarez, L., & Schreier, G. 2015. Personal Health Systems Technologies and Service Systems 2014. Presented at the 24th Annual RESER Conference, September 11–13, 2014, Helsinki, Finland